The Lab Mouse Paradox: Why Science Still Depends on Animals Who Don’t Represent Us
Despite significant advances in human-based research, millions of mice and rats are still used in U.S. laboratories each year—at immense ethical and scientific cost.
Introduction
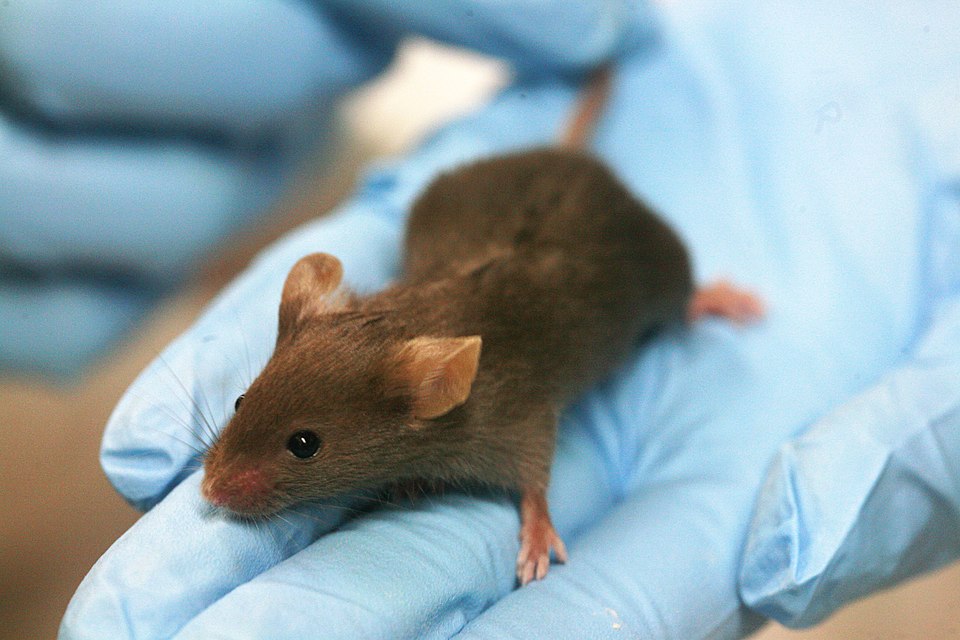
In the wild, a mouse or rat leads a precarious life. In the city, they dodge traps, poisons, and broom-wielding humans. In the countryside, they face owls, shotguns, and more poison. As Australia’s deputy prime minister once declared during a nationwide mouse plague, “The only good mouse is a dead mouse.” Yet even that grim existence might be preferable to the fate of those born in cages—bred by the millions each year for use in laboratories across the United States.
More than 111 million mice and rats are used, abused, and killed annually in biomedical research in the U.S. alone. These highly intelligent rodents account for 99 percent of all laboratory animals, but they have no legal protection under the federal Animal Welfare Act (AWA), which excludes them entirely from its definitions of covered species. Much of this research is funded by taxpayers—over $16 billion a year—even though a majority of Americans oppose the use of animals in scientific research, according to surveys.
Sue Leary, president of the Alternatives Research and Development Foundation, calls the numbers alarming. “If the numbers are anywhere near correct, the amount of pain and suffering that’s occurring in these animals is completely unacceptable,” she said.
When the Model Doesn’t Match the Patient
Beyond the moral cost lies a scientific problem. Mice and rats are convenient and inexpensive to breed, but they are poor stand-ins for human biology. In a landmark 2004 study, biologists Javier Mestas and Christopher C.W. Hughes found that mice and humans have fundamentally different immune responses, making the animals unreliable predictors of human disease or drug effects, pointing out that, as “65 million years of evolution might suggest, there are significant differences” between mouse and human immune responses. “In many cases, not only [do] successful mouse therapies fail to work in the clinic, they actually have opposite effects in patients, leading to exacerbation of disease,” they wrote in a 2007 article in the Mouse in Biomedical Research.
These failures are not isolated. Decades of research have shown that many promising treatments for cancer, Alzheimer’s, and autoimmune diseases crumble when moved from mouse to human trials. The result is a vast expenditure of time, money, and lives—both animal and human—on models that too often mislead rather than illuminate.
Sentient Lives Behind the Lab Cage
For all their differences, rats and mice share more with us than most people imagine. Studies and firsthand accounts reveal that rats form emotional bonds, recognize individual humans, and even suffer from loneliness and grief. “Male rats will snuggle up for a cuddle and find contentment when they are curled up in a person’s lap,” according to the animal rights organization PETA. Females, they add, are equally affectionate—just more energetic and curious.
Dr. Larry Carbone, a veterinarian and animal welfare scholar, has estimated that if rodents experience pain and distress at rates comparable to other lab animals, about 44.5 million undergo potentially painful experiments each year. “Rodents’ capacity to experience significant pain and distress in experiments is no longer contested,” he writes. “It is time to revisit the adequacy of their welfare protections.”
When Animals Are Poor Proxies for Humans
Even beyond rodents, the premise of using animals as stand-ins for human biology is increasingly questioned. Dr. Aysha Akhtar, a neurologist and fellow at the Oxford Center for Animal Ethics, has argued that animal experimentation is both unreliable and outdated. “A growing body of scientific literature raises important concerns about its reliability and predictive value for human outcomes,” she writes in Cambridge Quarterly of Healthcare Ethics. “The unreliability of animal experimentation across a wide range of areas undermines scientific arguments in favor of the practice.”
This challenge has sparked a global push toward methods that are not only more humane but also more relevant to human health—such as cell-based models, organ-on-a-chip systems, and computer simulations.
Ethics in Practice: The Three Rs and Policy Shifts
Scientists and ethicists have long endorsed a guiding framework known as the “Three Rs”: replacement of animals with non-animal models, reduction of the number of animals used, and refinement of methods to minimize suffering. While these principles provide a foundation, meaningful change requires both scientific innovation and institutional commitment.
Federal agencies in the United States have taken steps to implement these principles. The FDA Modernization Act 2.0 (2023) removed the longstanding requirement for animal testing in new drug approvals, allowing human-relevant methods to be used instead. Building on this, the FDA developed a roadmap for preclinical research that encourages the use of New Approach Methodologies (NAMs), including organ-on-chip systems and computational models, to improve predictive accuracy while minimizing animal use.
The Environmental Protection Agency (EPA) initially committed to phasing out mammal testing by 2035, but that plan was reversed in 2021. In April 2025, however, EPA Administrator Lee Zeldin reinstated the phase-out plan, setting a goal to reduce mammal testing by 30 percent by 2025 and to eliminate it by 2035. This represents a renewed federal effort to reduce reliance on animal models while promoting alternative methods in chemical safety assessments.
At the federal level, in 2025, Health and Human Services Secretary Robert F. Kennedy Jr. has advocated for significant reductions in animal testing across NIH and FDA research programs, promoting the adoption of advanced human-relevant methods to replace animal models wherever feasible.
These shifts reflect a broader recognition that scientific progress and ethical responsibility can advance together: more predictive human-relevant methods can reduce suffering without compromising research outcomes.
A Future Beyond Animal Testing
Building on these scientific and ethical shifts, lawmakers have also turned their attention to industries outside biomedical research. One major front is cosmetics. Despite public opposition and the availability of advanced non-animal testing technologies, countless small animals—including mice, rabbits, and guinea pigs—are still used to test products like lipstick, lotion, and shampoo. These procedures, once considered standard, now appear increasingly antiquated in an age of organ-on-a-chip systems, 3D tissue models, and computer simulations.
In response, members of Congress introduced the Humane Cosmetics Act (H.R. 1657) in 2025, which seeks to prohibit cosmetic testing on animals and ban the sale of new products tested on them. The proposed law would also prevent companies from outsourcing animal testing to other countries, effectively closing a global loophole that allows cruelty to persist abroad. Advocates argue that this approach would not only align the United States with the more than 40 nations that have already banned such testing—including every member of the European Union—but also accelerate innovation in safer, human-relevant methods. As the bill’s supporters note, no one needs cruelty to look or feel beautiful; what the nation needs are scientific and ethical standards that reflect both compassion and progress.
Additionally, the Humane Research and Testing Act (HRTA, 2021), a bipartisan initiative, proposes creating a National Center for Alternatives to Animals in Research and Testing within the NIH to fund and train scientists in non-animal approaches. The legislation also mandates transparency around the number of animals used in federally funded research, providing accountability to taxpayers and the public.
“The bill has immense potential to tackle the problem of millions of animals used in wasteful and repetitive research,” says Citizens for Alternatives to Animal Research and Experimentation (CAARE), the group that helped draft the legislation. “But it needs more cosponsors.” Barbara Stagno, CAARE’s president, believes the HRTA could be transformative. “Science has advanced considerably in the 21st century so that research can be performed using non-animal methods that are more relevant to human medicine,” she told Earth | Food | Life. “Despite that, many millions of animals continue to be used. The Humane Research and Testing Act holds great promise to change that paradigm.”
In support of these efforts, Jane Goodall, the famed late primatologist, has spoken about the conditions she witnessed in research labs, calling them “shocking and unacceptable.” She emphasized that creating dedicated centers for non-animal research methods could lead to transformative change. Goodall’s testimony underscores the paradox at the heart of modern science: the animals most reviled as pests and most revered as research tools might also be among their most unnecessary casualties. As technologies advance and policies evolve, the question is no longer whether we can replace animal testing—but whether we will.